Technology & Innovations
Neural Implants for Pain Management: Exploring the Potential of Brain Implants
Imagine a world where chronic pain no longer dictates your life, where relief is not just a temporary fix but a permanent solution.
Neural implants offer a glimmer of hope in this realm, promising a future where pain management is revolutionized.
In this blog post, we will discuss the fascinating world of neural implants for pain management, exploring how this groundbreaking technology is reshaping the way we perceive and treat chronic pain.
Key Takeaways
- Neural Implants Revolutionizing Pain Management: Implants offer hope for chronic pain sufferers, potentially reshaping treatment approaches.
- Chronic Pain Overview: Understand the causes, symptoms, and impact on quality of life to appreciate the need for innovative solutions.
- Science Behind Neural Implants: Explore how different types of implants work to disrupt pain signals and provide relief.
- Benefits and Challenges: Weigh the advantages of precise targeting and long-term pain management against potential risks and ethical concerns.
- Future of Pain Relief: Advancements in neural implant technology offer a promising future for personalized and effective pain management.
TL;DR
Neural implants are emerging as a promising solution for chronic pain management. They work by modulating pain signals in the brain or nervous system, offering an alternative to traditional treatments.
While the technology is still evolving, successful cases highlight its potential to improve quality of life for those suffering from chronic pain.
Advancements in neural implants, combined with other therapies, hold the key to a future where pain relief is more effective and personalized.
Table of Contents
Neural Implants and Their Role in Pain Management

Let’s start by discussing the concept of neural implants and their crucial role in managing pain.
Neural implants, also known as brain implants or neurostimulators, are electronic devices designed to directly stimulate the nervous system to modulate the perception of pain.
These innovative devices can be surgically implanted in specific areas of the brain or spinal cord to disrupt pain signals and provide relief to individuals suffering from chronic pain conditions.
Imagine having a tiny device implanted in your body that can effectively alleviate your pain without the need for constant medication.
Neural implants offer a promising alternative for individuals who have exhausted traditional pain management methods and are seeking long-term relief.
Brief History and Evolution of Neural Implant Technology
The evolution of neural implant technology is nothing short of remarkable.
The roots of neural implants can be traced back to the early 20th century when scientists began exploring the electrical stimulation of the nervous system for therapeutic purposes.
Over the decades, advancements in medical technology and neuroscience have paved the way for the development of sophisticated neural implant devices that are more precise and effective in targeting pain pathways.
From the first simple experiments with electrical stimulation to the cutting-edge neurostimulators available today, the field of neural implant technology has witnessed rapid progress and significant breakthroughs.
Researchers and engineers continue to push the boundaries of innovation, enhancing the safety and efficacy of neural implants for pain management.
Current Landscape of Pain Management and the Need for Innovative Solutions
The current landscape of pain management is fraught with challenges, with millions of people worldwide enduring chronic pain that significantly impacts their quality of life.
Traditional pain management approaches, such as medication and physical therapy, may provide temporary relief but often come with side effects and limitations.
It is in this backdrop that the need for innovative solutions like neural implants becomes increasingly evident.
By targeting the neural pathways responsible for transmitting pain signals, neural implants offer a novel approach to managing chronic pain conditions more effectively and sustainably.
As research in this field progresses and technology advances, we are witnessing a shift towards personalized and precision medicine in pain management.
We’ll explore the latest advancements, clinical applications, and future prospects in the next sections of this blog.
Understanding Chronic Pain and Current Treatment Methods

Dealing with chronic pain can be a real struggle, impacting every aspect of your life.
Next, we’ll discuss the causes, symptoms, and the effect it has on your overall quality of life.
We will also explore the commonly used medications and therapies for chronic pain, as well as the limitations and drawbacks that come with traditional pain management approaches.
Overview of Chronic Pain
Chronic pain is more than just a regular ache or discomfort. It persists for weeks, months, or even years, affecting your daily activities and mental well-being.
The causes of chronic pain can vary widely, from underlying medical conditions to injuries or surgeries that never fully heal.
Common symptoms of chronic pain include sharp or dull aching, shooting or burning sensations, stiffness, and limited mobility.
These symptoms not only affect you physically but can also take a toll on your emotional and mental health, leading to increased stress, anxiety, and depression.
Medications and Therapies for Chronic Pain
There are various treatment options available to manage chronic pain. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and opioids are commonly prescribed to help alleviate pain.
However, long-term use of opioids can lead to dependency and other adverse effects, making them a controversial choice for chronic pain management.
Aside from medications, there are also non-pharmacological approaches to consider.
Physical therapy, acupuncture, massage therapy, and cognitive-behavioral therapy are just a few examples of alternative therapies that can help manage chronic pain.
These methods focus on improving physical function, reducing pain levels, and enhancing overall well-being.
Limitations of Traditional Pain Management Approaches
While traditional pain management approaches have their benefits, they also come with limitations and drawbacks.
For instance, medications only provide temporary relief and may not address the root cause of the pain. Moreover, long-term use of certain medications can result in side effects and complications.
Similarly, relying solely on therapies like physical therapy or acupuncture may not provide long-lasting relief for chronic pain. It often requires a combination of treatments tailored to your specific condition and needs to effectively manage pain in the long term.
It’s essential to work closely with healthcare providers to develop a comprehensive pain management plan that accounts for both the physical and emotional aspects of chronic pain.
The Science Behind Neural Implants: How Do They Work?

Have you ever wondered how neural implants work and what makes them such a groundbreaking technology in the field of pain management?
Let’s dive into the fascinating world of neural implants and explore their mechanism of action and the different types used for pain management.
Explanation of Neural Implants and Their Mechanism of Action
As mentioned earlier, neural implants, also known as brain implants or brain-computer interfaces, are devices that are surgically implanted into the brain to help restore or enhance neural functions.
These implants work by directly interfacing with the brain’s neural circuits, allowing for the exchange of electrical signals between the device and the brain.
Neural implants can help treat a variety of neurological conditions, including chronic pain, Parkinson’s disease, epilepsy, and spinal cord injuries by detecting and modulating neural activity.
The key to their functionality lies in their ability to decode and interpret neural signals, enabling them to deliver targeted stimulation to specific areas of the brain.
Types of Neural Implants Used for Pain Management
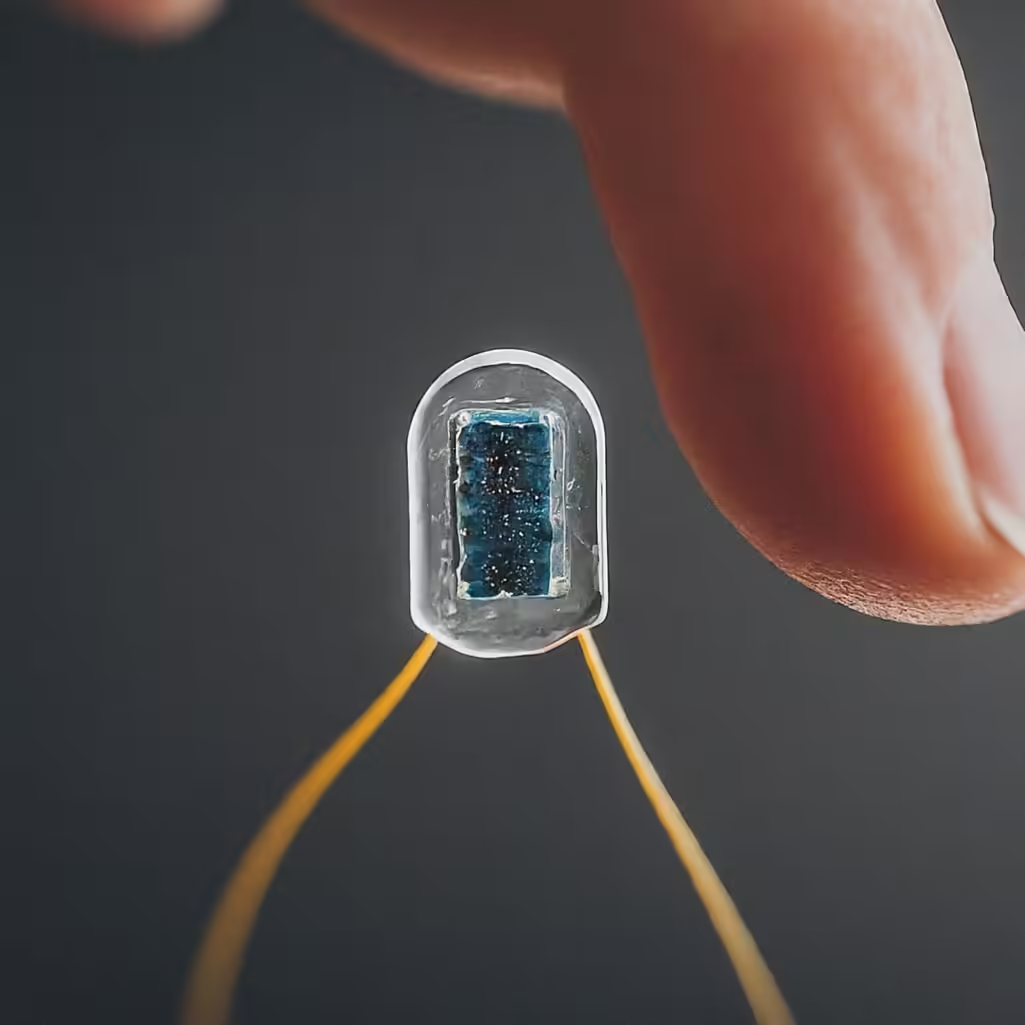
There are several types of neural implants that are commonly used to treat chronic pain, each with its unique mechanism of action and benefits.
- Spinal Cord Stimulators: These implants deliver electrical pulses to the spinal cord, disrupting pain signals and providing relief for individuals suffering from chronic back pain or neuropathic pain.
- Deep Brain Stimulators: By targeting specific areas of the brain involved in pain processing, deep brain stimulators can help alleviate chronic pain conditions such as cluster headaches and neuropathic pain.
- Vagus Nerve Stimulators: These implants stimulate the vagus nerve, which plays a key role in regulating pain perception and inflammation, offering relief for conditions like migraines and fibromyalgia.
Top 5 Neural Implants for Pain Management in 2024:
Spinal Cord Stimulation (SCS):
- Benefits: Effective for chronic back pain, neuropathic pain, and failed back surgery syndrome. Customizable stimulation patterns for personalized relief.
- Pros: Minimally invasive procedure, reversible, adjustable settings for optimal pain control.
- Cons: Risk of infection, lead migration, battery replacement surgery, not suitable for all types of pain.
Deep Brain Stimulation (DBS):
- Benefits: For Parkinson’s disease, essential tremor, and dystonia. Potential for treating chronic pain, depression, and OCD.
- Pros: Significant improvement in motor symptoms and quality of life, adjustable settings for personalized therapy.
- Cons: Invasive brain surgery, risk of infection, bleeding, and hardware malfunction, requires ongoing programming adjustments.
Vagus Nerve Stimulation (VNS):
- Benefits: FDA-approved for epilepsy and treatment-resistant depression. Emerging evidence for chronic pain, migraines, and inflammatory conditions.
- Pros: Minimally invasive procedure, adjustable stimulation parameters, potential for broad therapeutic applications.
- Cons: Risk of hoarseness, cough, and throat discomfort, not suitable for all patients, long-term efficacy data still emerging.
Peripheral Nerve Stimulation (PNS):
- Benefits: Targets specific nerves for localized pain relief in conditions like migraines, pelvic pain, and post-surgical pain.
- Pros: Minimally invasive procedure, reversible, adjustable stimulation for personalized pain control.
- Cons: Risk of infection, lead migration, limited long-term data, not suitable for all types of pain.
Dorsal Root Ganglion Stimulation (DRG):
- Benefits: Specifically targets pain signals from a particular area of the body, effective for localized neuropathic pain syndromes.
- Pros: Minimally invasive procedure, reversible, high patient satisfaction rates for targeted pain relief.
- Cons: Limited long-term data, risk of infection, lead migration, not suitable for widespread pain.
Neural implant technology is rapidly evolving, and new devices are constantly being developed.
As always, consult with a qualified healthcare professional to determine the most appropriate neural implant for your specific condition and needs.
Benefits and Challenges of Using Neural Implants for Pain Management
So, what are the advantages, potential risks, and benefits of neural implants?
Advantages of Neural Implants over Traditional Pain Medications
Neural implants offer a promising alternative to traditional pain medications for managing chronic pain.
Here are some key advantages that neural implants bring to the table:
- Precision Targeting: Neural implants can directly target specific areas of the brain associated with pain perception, providing more targeted and effective pain relief compared to systemic medications.
- Long-Term Pain Management: Unlike temporary relief provided by pain medications, neural implants have the potential to provide long-term pain management solutions, reducing the need for frequent medication intake.
- Improved Quality of Life: By effectively managing chronic pain, neural implants can significantly improve an individual’s quality of life, allowing them to engage in daily activities with reduced discomfort.
- Reduced Dependency on Drugs: Neural implants may lessen the reliance on opioid and other pain medications, potentially minimizing the risk of dependency and addiction.
Potential Risks and Side Effects Associated with Neural Implant Surgery
While neural implants hold promise for pain management, it is essential to consider the potential risks and side effects associated with the surgical implantation process.
Some of the risks include:
- Surgical Complications: As with any surgical procedure, there is a risk of complications such as infection, bleeding, or adverse reactions to anesthesia.
- Device Malfunction: Neural implants may pose a risk of device malfunction or failure over time, requiring monitoring and possible replacement of the implant.
- Psychological Impact: The implantation process and adjustment to having a neural implant may have psychological implications for some individuals, necessitating proper counseling and support.
- Regulatory Concerns: Regulatory challenges and ethical considerations surrounding neural implants raise questions about data privacy, consent, and long-term safety monitoring.
Ethical Considerations and Future Implications of Widespread Neural Implant Use
As neural implants become more prevalent in pain management, it’s important to address the ethical considerations and anticipate future implications of their widespread use:
- Privacy and Data Security: Ensuring patient data privacy and protection from potential breaches or misuse of neural implant technology is paramount in ethical implementation.
- Equitable Access: Striving for equitable access to neural implant technology to ensure that all individuals in need have the opportunity to benefit from advanced pain management solutions.
- Long-Term Outcomes: Continued research and monitoring are essential to assess the long-term effects of neural implants on patients’ overall health, well-being, and quality of life.
- Collaborative Approaches: Encouraging collaboration between healthcare providers, researchers, ethicists, and regulatory bodies can facilitate responsible and ethical development and implementation of neural implant technology.
The Future of Pain Relief: Implications and Possibilities
Imagine a world where chronic pain could be managed more effectively, giving hope to millions of individuals seeking relief.
The future of pain treatment holds exciting possibilities, with advancements in neural implant technology leading the way.
Here are some key talking points that shed light on the potential implications and possibilities that neural implants offer for pain management:
Emerging Trends and Advancements in Neural Implant Technology
Neural implant technology has come a long way in recent years, with innovations that have the potential to revolutionize the field of pain management.
These implants work by stimulating specific areas of the brain or nervous system to modify pain signals, providing relief to individuals suffering from chronic conditions.
The development of smaller, more efficient implantable devices is enabling greater precision and customization in targeting pain pathways.
Researchers are continually exploring new materials and techniques to improve the efficacy and longevity of these implants, paving the way for more effective pain relief strategies.
Integration of Neural Implants with Other Pain Management Strategies

While neural implants show promise as standalone pain management solutions, their true potential lies in integration with other treatment modalities.
Combining neural implants with therapies such as medication, physical therapy, or cognitive-behavioral approaches, can offer healthcare providers more comprehensive and personalized care to patients.
This integrated approach allows for a multidimensional treatment plan that addresses both the physical and psychological aspects of pain, leading to improved outcomes and enhanced quality of life for individuals living with chronic pain conditions.
Predictions for the Future of Pain Treatment and Quality of Life Improvements
Looking ahead, the future of pain treatment holds exciting possibilities for individuals seeking relief from debilitating conditions.
As neural implant technology continues to advance, we can expect to see increasingly sophisticated devices that offer greater precision and effectiveness in targeting pain signals.
These advancements have the potential to not only alleviate pain symptoms but also enhance overall quality of life for patients.
With improved treatment strategies and a more holistic approach to pain management, individuals suffering from chronic pain can look forward to a future with greater comfort and well-being.



